Hearing that you have an ovarian cyst can feel unsettling, especially when you are unsure what it means for your health or fertility. The good news is that most cysts are benign and many disappear on their own without any need for surgery. When a cyst causes symptoms, grows larger, or looks suspicious on a scan, your doctor may recommend removal. Today, laparoscopy for ovarian cysts has become the preferred approach for many women because it uses small cuts, leads to less pain, and allows a faster recovery than traditional open surgery.
Choosing the right ovarian cyst treatment depends on your symptoms, scan findings, age, and plans for future pregnancy. This guide explains ovarian cyst symptoms, how doctors decide on treatment, what to expect from ovarian cyst surgery by laparoscopy, and how to choose the best gynecologist for ovarian cysts in Dubai.
Ovarian cysts in everyday language
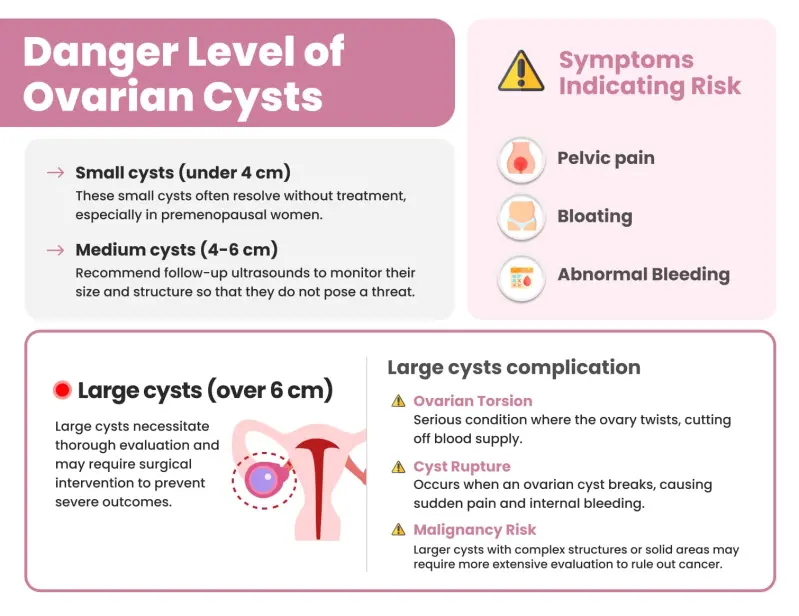
An ovarian cyst is a fluid-filled sac that forms in or on the ovary. Functional cysts appear as part of the normal cycle and often melt away within a few months. Others, like endometriomas related to endometriosis, dermoid cysts, or cystadenomas, are nonfunctional and may persist or grow. Most cysts are not cancerous, and before menopause, the risk of cancer is low, although it is never zero. Many women only discover a cyst during a routine ultrasound and feel completely well. When cysts do cause problems, they can lead to pelvic pressure, bloating, pain that worsens around the period, pain during intimacy, or pain on one side that waxes and wanes. Sudden severe pain with nausea can occur if a cyst twists the ovary or ruptures, which requires urgent assessment.
In many cases, the safest plan is to watch and wait with repeat scanning over several weeks because functional cysts frequently resolve. Large or persistent cysts, cysts that cause ongoing pain, and cysts with features that do not look benign on ultrasound are more likely to need surgery. Authoritative patient resources confirm that most cysts are harmless and that watchful waiting is often appropriate, with surgery reserved for specific situations.
Why is laparoscopy often the first choice
Laparoscopy is a keyhole technique that uses a thin camera and fine instruments inserted through tiny cuts in the abdomen. For many women, it has clear advantages over a larger open cut. Recovery is quicker, there is less pain after surgery, and hospital stays are shorter. National guidance for patients explains that when surgery is needed, a laparoscopic approach is preferred in suitable cases, and many women go home the same day or the day after.
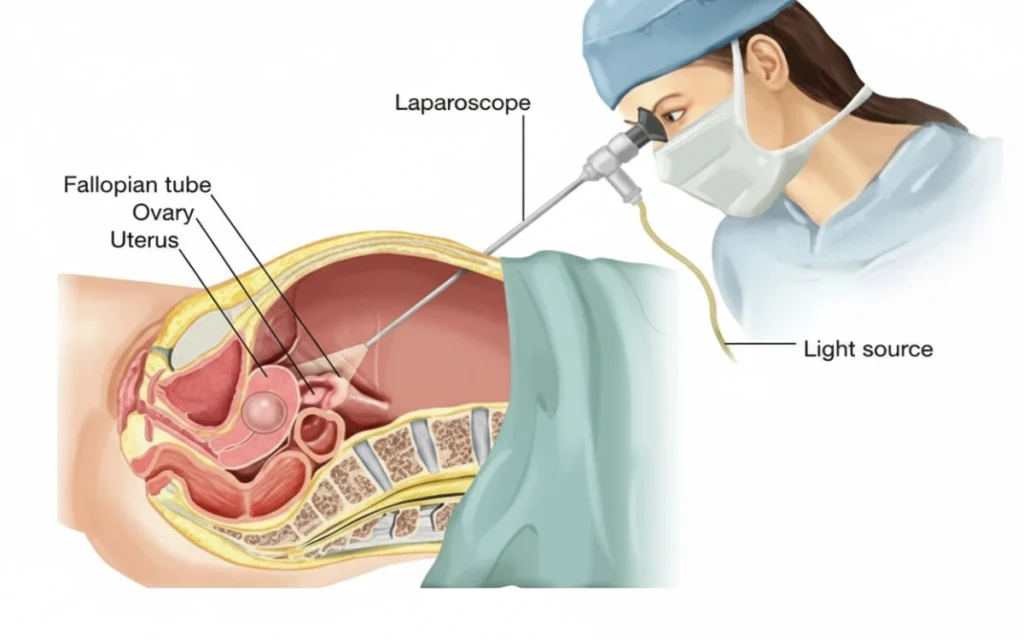
The surgeon’s goals are to remove the cyst safely, preserve as much healthy ovarian tissue as possible, and reduce the chance of cysts returning. Preserving ovarian tissue matters for future hormone balance and fertility. During laparoscopy, surgeons usually perform a cystectomy, which means peeling the cyst capsule away from the ovary and repairing the surface. If the cyst is too large, severely damaged, or suspicious for malignancy, a different plan may be advised. Medical organisations note that if a mass looks worrisome for cancer on the scan, shows a concerning blood marker pattern, or raises red flags on examination, open surgery and involvement of a gynaecologic oncologist are recommended rather than laparoscopy.
How doctors decide on ovarian cyst treatment
Selecting the right ovarian cyst treatment begins with a careful history and examination. Your doctor will ask about pain patterns, cycle changes, family history, and fertility plans. A transvaginal ultrasound gives the most useful details about the cyst’s size, wall thickness, internal echoes, and blood flow. Blood tests may include haemoglobin if bleeding is heavy and CA-125 in selected scenarios, especially after menopause. Patient leaflets from professional colleges explain that cysts before menopause are commonly benign and many do not require immediate intervention, while specific algorithms guide next steps in postmenopausal women, where the approach is more cautious.
When surgery is recommended, your team will discuss whether to plan a laparoscopic cystectomy or a different operation. Laparoscopy is often chosen for benign appearing cysts because it provides excellent visualisation and allows precise removal through tiny incisions. Reputable clinical guidance for patients and clinicians describes laparoscopy as an effective method to both diagnose and treat cysts in the same sitting.
What does a laparoscopy for ovarian cysts involve
Laparoscopic surgery is performed under general anaesthesia. Through a small cut near the navel, the abdomen is gently inflated to create working space. A camera is inserted to inspect the pelvis. Two or three additional tiny cuts allow the instruments to remove the cyst. If the cyst contains thick fluid or solid tissue, it is placed in a bag before removal to prevent spillage. The surgeon then checks for bleeding, washes the area, and closes the skin with dissolvable stitches. The cyst is sent to the laboratory for confirmation of the diagnosis.
The operation time varies with cyst size and type. In straightforward cases, the procedure is usually short, and many women leave the hospital the same day once they are comfortable and drinking and walking. Authoritative NHS guidance notes that laparoscopy generally causes less pain and allows return home within hours or by the next day.
Recovery and return to normal life
Most patients feel shoulder tip discomfort from the gas used to inflate the abdomen, which settles within a day or two as the gas is absorbed. Light activities are encouraged early, and gentle walking helps circulation and reduces stiffness. Tiredness is common for a few days and improves with rest, hydration, and small, frequent meals. Trusted hospital resources suggest that many women return to desk-based work within one to two weeks after laparoscopic cystectomy, while strenuous activity and heavy lifting typically wait a little longer. Recovery after open surgery takes longer because the cut is larger and muscle layers need more healing time, often several weeks.
Your team will let you know about showering, wound care, and when to resume exercise and intimacy. A follow up visit is usually arranged to review the pathology report and talk through any further care. If you experience fever, increasing abdominal pain, heavy bleeding, calf swelling, or shortness of breath, you should contact your doctor promptly.
Safety profile and possible risks
Even keyhole procedures carry risks, although serious complications are uncommon in healthy women. Possible problems include bleeding, infection, injury to nearby organs, and adverse reactions to anaesthesia. Blood clots can occur but are rare in short laparoscopic procedures and can be further reduced by early mobilisation and preventive measures in the hospital. Reputable patient information explains these risks clearly so you can give informed consent and feel confident about what to expect.
A special note about cancer risk is important. When ultrasound and blood markers suggest a mass may be malignant, the plan usually changes. In such cases, open surgery by a specialist cancer surgeon allows careful staging and the safest technique for removal. Clinical summaries of expert guidance emphasise that laparoscopy is not the first choice for masses that appear suspicious for cancer.
Laparoscopy versus laparotomy in plain terms
Laparoscopy uses small incisions and a camera, while laparotomy uses a larger cut to open the abdomen. For benign ovarian cysts, laparoscopy generally offers faster recovery, less pain, and fewer adhesions. It also results in smaller scars and a quicker return to work and exercise. Open surgery is still the right choice in certain situations, such as very large cysts that cannot be removed safely through small cuts, significant scarring from previous operations, or when the cyst looks suspicious for malignancy on the scan. Well-regarded patient and clinician resources describe laparoscopy as effective for benign disease and open surgery as safer for suspected cancer.
Fertility and ovarian preservation
For many women, protecting fertility is a central concern. During ovarian cyst surgery, the priority is to remove the cyst while preserving healthy ovarian tissue. Laparoscopic cystectomy is designed for that goal. In women with endometriomas or recurrent cysts, your surgeon will balance the benefits of cyst removal against the small risk of reducing ovarian reserve. This is why choosing an experienced surgeon matters. High-quality patient information explains that laparoscopy can both diagnose and treat in one procedure and that most premenopausal cysts are benign, allowing a conservative and fertility-aware plan.
If you are not ready to conceive, your doctor can discuss methods to reduce recurrence, such as hormonal suppression in selected cases. If you are planning a pregnancy soon, removing a painful or persistent benign cyst can improve comfort and may make fertility treatment, if needed, safer and simpler.
Special considerations after menopause
Cysts after menopause require a different decision pathway. Even though many postmenopausal cysts are still benign, doctors use a structured approach that includes ultrasound features and blood markers. Some simple cysts can be monitored safely with repeat scans and a normal CA-125. Others are better managed with surgery due to a higher risk of malignancy in this age group. Professional guidelines outline when to observe and when to operate so women receive care that is both safe and proportionate.
When laparoscopy may not be recommended
Your doctor may advise an alternative to laparoscopy if you have severe heart or lung disease that makes gas insufflation unsafe, extensive scar tissue from previous operations that raises the risk of organ injury, very large masses that will not fit through small incisions, or any features that increase concern for cancer. In pregnancy, laparoscopy can be performed safely in selected cases by experienced teams, although timing and technique are adjusted with the obstetric team’s input. Decisions are made on a case-by-case basis to protect both mother and baby. Studies and reviews suggest laparoscopy can offer advantages even during pregnancy when used appropriately.
Frequently asked questions
How do I know if my cyst needs surgery or can be watched?
This depends on your symptoms, the cyst’s appearance and size on ultrasound, your age, and whether you are pregnant. Many functional cysts disappear within a few months and can be safely monitored. Surgery is more likely if the cyst is large, painful, persistent, or has complex features. Well-regarded patient resources support this watchful waiting approach for many women.
Is laparoscopy always better than open surgery?
For benign appearing cysts, laparoscopy usually means less pain, shorter hospital stay, and quicker return to normal life. Open surgery remains the safer option when the cyst looks suspicious for cancer or when a very large mass cannot be removed through small cuts.
How long will I take to recover after laparoscopic cyst removal?
Most women resume light activities within several days and return to desk work within one to two weeks. Full recovery after open surgery can take much longer because of the larger cut. Recovery is personal, and your surgeon will tailor advice to your situation.
What risks should I know about?
All operations carry risks such as bleeding, infection, injury to nearby organs, and blood clots, but serious complications are uncommon in straightforward laparoscopic procedures. Your team will discuss your individual risk and the steps taken to reduce it.
Will removing the cyst affect my fertility?
The goal of cystectomy is to remove the cyst and preserve the ovary. Skilled laparoscopic technique focuses on minimising heat or trauma to healthy tissue. Your surgeon will discuss how cyst type and size influence the plan and any implications for ovarian reserve. Authoritative sources highlight the role of laparoscopy in treating benign cysts while protecting ovarian function when possible.
Choosing the best gynecologist for ovarian cysts in Dubai
Selecting the best gynecologist for ovarian cysts is about experience, communication, and access to a modern surgical setup. You should feel heard during your consultation and fully informed about your options. Your surgeon should be comfortable performing both laparoscopy and open procedures and willing to work alongside a gynaecologic oncologist if scan features raise concern. A centre with high-quality imaging, anaesthesia support, and day surgery facilities makes your journey smoother and safer.
A note from Dr. Neha Lalla
Most ovarian cysts can be managed conservatively, and when surgery is needed, laparoscopy offers a safe and effective solution for many women. My approach is to personalise care, protect fertility, and plan surgery only when the benefits clearly outweigh the risks. If you have pelvic pain, a newly diagnosed cyst, or a cyst that has not resolved with observation, a focused consultation can bring clarity and a plan that fits your goals.
Conclusion
Laparoscopy has reshaped ovarian cyst treatment by offering small incisions, less pain, and a quicker return to normal life for appropriately selected patients. It is not the only option, and it is not right for every cyst, but it is often the safest and most comfortable path when a benign cyst needs to come out. Understanding your scan, your symptoms, and your priorities helps your doctor guide you toward the right decision.
If you live in Dubai and have questions about laparoscopy for ovarian cysts or want an expert second opinion on ovarian cyst surgery, book a consultation with Dr. Neha Lalla. Together you can review your images, discuss risks and benefits, and choose a plan that supports your health and future fertility.


