Pregnancy is a remarkable season of life, yet it sometimes needs closer attention to keep mother and baby safe. When doctors use the term high-risk pregnancy, it means extra care is needed because certain factors could increase the chance of complications. A high-risk label is not a prediction of a poor outcome. It is a prompt to take a more attentive approach. With the right team, the right plan, and timely reviews, most women with a high-risk pregnancy deliver healthy babies and recover well.
Knowing the signs of high-risk pregnancy and understanding how specialist care works can remove uncertainty and help you feel prepared. This guide explains what places a pregnancy in the high-risk category, how maternal fetal medicine specialists support you, and which steps reduce risk from the first trimester through birth. If you are in Dubai and looking for a high-risk pregnancy specialist, you will also learn how expert care is organised locally so you can navigate appointments with confidence.
What “high-risk pregnancy” really means
High-risk pregnancy is a practical label that helps clinicians plan closer monitoring and targeted care. Sometimes the reason is present before conception, such as type 1 diabetes, high blood pressure, thyroid disease, kidney disease, an autoimmune condition, or a history of surgery on the uterus. Sometimes the reason is identified during pregnancy, such as gestational diabetes, pregnancy-induced hypertension, a short cervix, placenta previa, growth restriction, or twins and higher order multiples. Maternal age under 18 or over 35 can shift a pregnancy into a closer-watch category, as can previous pregnancy complications like preeclampsia, preterm birth, recurrent pregnancy loss, or a baby affected by a genetic or structural condition.
The common thread is the need for more information and more touchpoints. Extra scans, focused blood tests, and planned reviews allow your team to spot small changes early and act before problems escalate. This is the heart of modern care for pregnancy complications. It is proactive rather than reactive.
Why this topic matters in Dubai

Women in Dubai enjoy access to advanced imaging, laboratory services, and hospital facilities, which makes expert management of high-risk pregnancy both practical and effective. The pace of professional life can be demanding, travel schedules can be dense, and many families live far from extended relatives. These realities make structured support even more valuable. A clear schedule, accessible communication, and practical guidance on work, exercise, fasting during religious seasons, and travel planning help you protect your health while meeting daily responsibilities.
Climate is another consideration. Warm weather increases daily fluid requirements, and dehydration can worsen headaches, raise heart rate, and trigger contractions in sensitive periods. Women with high-risk pregnancies should plan hydration carefully and discuss suitable activity levels with a specialist. Dubai also serves a multicultural population, which means nutritional habits, genetic backgrounds, and health beliefs vary widely. A high-risk pregnancy specialist will tailor advice to your language, culture, and family context, so that recommendations are both safe and realistic.
Signs of high-risk pregnancy you should not ignore
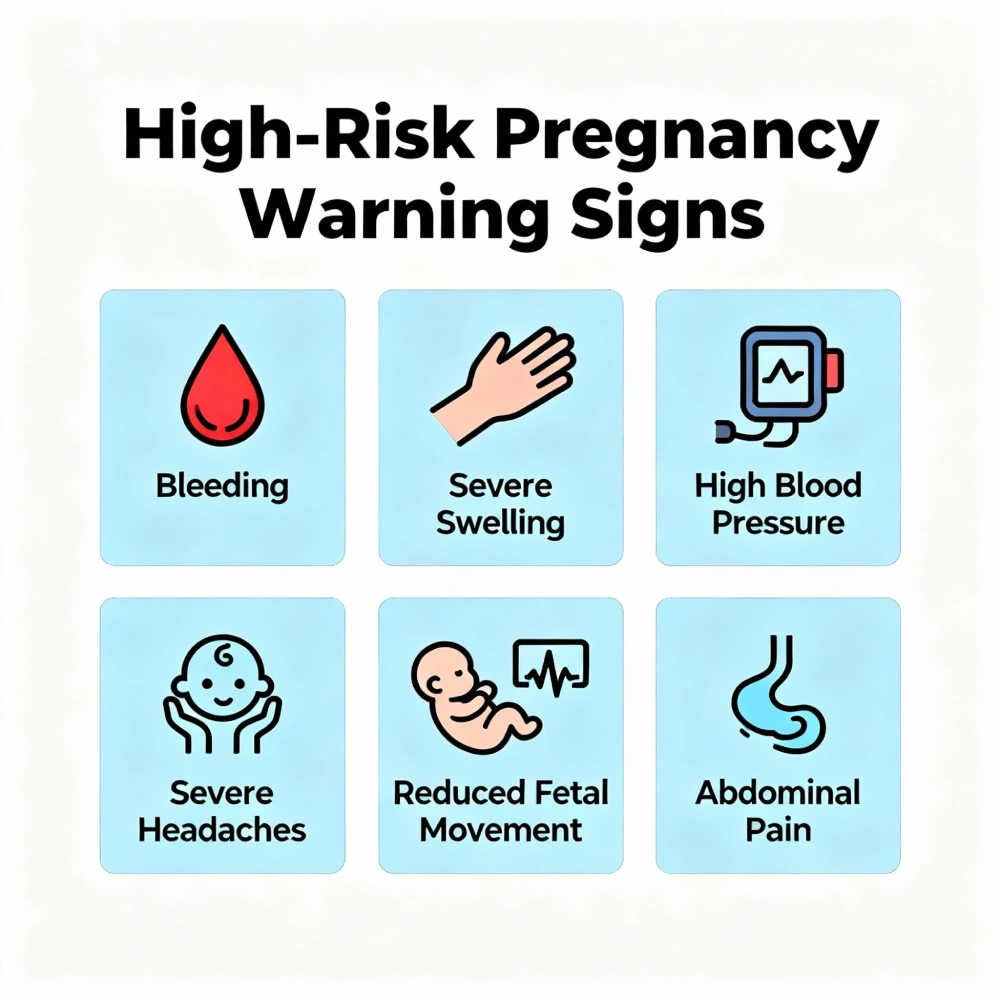
Many women feel well throughout pregnancy, even when risk factors are present. That said, certain warning signs deserve immediate attention. Vaginal bleeding, a gush or persistent leak of fluid suggesting ruptured membranes, painful contractions before 37 weeks, a sudden severe headache, visual disturbances, intense pain below the ribs on the right, sudden swelling of the face or hands, breathlessness at rest, chest pain, fever, or a noticeable reduction in baby’s movements after 28 weeks should prompt a call to your doctor or a visit to the hospital. These signs do not always mean a serious problem is present, but they are the signals that maternal fetal medicine teams want to assess without delay.
There are quieter signals as well. Persistent vomiting that limits fluid intake, blood pressure readings that trend upward at home, fasting or post-meal sugars outside targets if you have diabetes, or home urine checks showing protein when you have hypertension all indicate the need for review. Trust your instincts. If something feels different or worrisome, seek advice. Early contact often prevents overnight stays and keeps the plan simple.
How maternal fetal medicine supports you
Maternal fetal medicine is a subspecialty of obstetrics that focuses on high-risk pregnancy and pregnancy complications. A maternal fetal medicine specialist works alongside your primary obstetrician to provide advanced scanning, risk assessment, and treatment planning. The partnership can be brief, such as a single detailed anatomy scan, or ongoing, such as shared care for preeclampsia, growth restriction, or twins.
At your first high-risk consultation, the specialist reviews your history, medications, previous pregnancy outcomes, and family background. You will discuss lifestyle factors, work duties, travel plans, and any cultural or religious practices that could influence care. The doctor will map out a surveillance plan that might include targeted ultrasound for structural review, cervical length measurement in the mid-trimester if indicated, uterine artery Doppler studies for early placental assessment, and growth scans to track the baby’s development. Later in pregnancy, you may have non-stress tests and biophysical profiles, which assess heart rate patterns, movement, tone, breathing movements, and amniotic fluid. The goal is to answer three questions at each visit: how are you, how is the placenta, and how is the baby growing and coping. Clear answers to those questions allow safe decisions about timing and mode of birth.
The investigations you may encounter
The workup for a high-risk pregnancy is guided by your individual needs rather than a fixed list. If high blood pressure is present or suspected, you may be given a home monitor and taught how to record readings correctly. Blood tests will check kidney and liver function, platelets, and markers that help identify preeclampsia early. If gestational diabetes is a concern, a glucose tolerance test or continuous glucose monitoring may be advised. Thyroid function is checked when symptoms, history, or early losses point to a possible imbalance. If your body mass index is high, screening for vitamin D deficiency and careful dose planning for supplements can support both maternal and fetal bone health.
Ultrasound plays a central role. A detailed anatomy scan at the mid-trimester assesses the baby’s organs from head to toe. If the cervix measures short, vaginal progesterone or a cervical stitch may be discussed to reduce the risk of preterm birth. If the placenta sits low, follow-up scans track its movement as the uterus grows. In growth restriction, Doppler blood-flow studies in the umbilical artery and middle cerebral artery help decide how closely to monitor and when to deliver. None of these tests is performed for its own sake. Each one helps with a real decision, such as adjusting medication, admitting for observation, or planning the timing of birth.
Treatment pathways that reduce risk
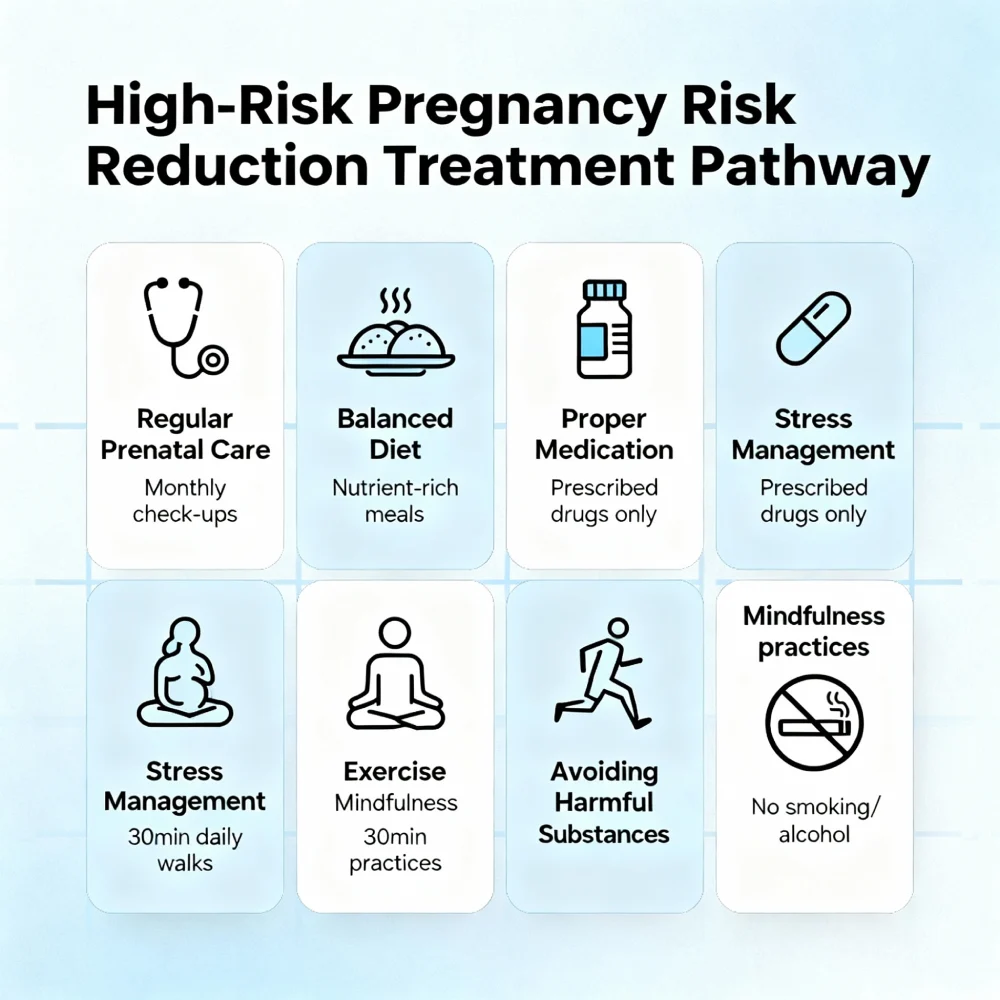
Treatment in high-risk pregnancy focuses on maintaining stable maternal health, supporting the placenta, and choosing the safest moment for birth. If you have chronic hypertension, pregnancy-safe blood pressure medicines keep readings in the target range and reduce the chance of severe spikes. If you are at higher risk of preeclampsia, your specialist may recommend low-dose aspirin from early pregnancy until near delivery. In diabetes, a combination of tailored nutrition advice, activity planning, and medication when needed keeps glucose in range and lowers the risk of excessive fetal growth and birth complications. Thyroid conditions are managed with careful dosing to protect neurodevelopment.
Preterm birth prevention is a priority when the cervix is short or the history includes early delivery. Vaginal progesterone, cervical cerclage, or both may be used depending on the scenario. If the risk of early delivery rises, two doses of corticosteroids given 24 hours apart accelerate the baby’s lung maturity. Magnesium sulphate can protect the baby’s brain if birth is expected before 32 to 34 weeks. These decisions are time sensitive, which is why frequent reviews are part of a high-risk plan.
Multiple pregnancy care is tailored to whether twins share a placenta. Monochorionic twins require closer ultrasounds because they face distinct risks, while dichorionic twins may follow a less intensive schedule. In growth restriction, careful timing balances the benefit of staying in the womb against the risk of placental insufficiency. When the scales tip, your team will recommend delivery in a hospital with neonatal support.
Everyday steps you can take
Specialist care is vital, yet daily habits carry real weight. A balanced diet that includes vegetables, fruit, whole grains, lean protein, healthy fats, and adequate calcium supports both mother and baby. Hydration deserves special care in Dubai. Keeping a water bottle at hand and setting reminders to drink can steady energy and reduce headaches. Light activity, such as walking or prenatal yoga, helps circulation and sleep unless your specialist has asked you to limit exertion. Rest is not laziness in a high-risk pregnancy. It is therapy. Prioritise sleep, plan short breaks during the day, and ask for help with tasks that add strain.
Avoiding smoking and alcohol is essential. Review all medicines and supplements with your doctor. Immunisations such as influenza and pertussis are routinely recommended during pregnancy to protect both mother and newborn. Mental health is health. If anxiety or low mood surfaces, share this with your team. Support can include counselling, peer groups, or safe medication when indicated. An emotional plan is as important as a medical one.
Planning birth with a high-risk pregnancy specialist
Birth planning is not a single meeting. It is a rolling conversation shaped by scan findings, test results, symptoms, and your preferences. Some high-risk pregnancies are well suited to vaginal birth, while others clearly benefit from a planned caesarean. Timing is customised. Women with uncomplicated gestational diabetes may aim for delivery near their due date. Women with growth restriction, poorly controlled hypertension, or cholestasis may be advised to deliver earlier. If a baby is expected to need support after birth, delivery is planned in a hospital with a neonatal unit. The presence of a high-risk pregnancy specialist ensures a calm, coordinated approach that minimises last-minute surprises.
After birth, attention does not end. Blood pressure often peaks in the first week postpartum. Diabetes control changes rapidly when the placenta is delivered. Caesarean wounds and perineal repairs need assessment. Breastfeeding support and mental health check-ins are part of a complete plan. A final postpartum review brings the story together and sets you up for future pregnancies with knowledge and confidence.
Frequently asked questions
Does a high-risk pregnancy always mean a caesarean birth?
No. Many women with high-risk pregnancies give birth vaginally. The decision depends on the specific condition and how the mother and baby are coping. Your specialist will explain the safest route and timing based on updated assessments rather than a one-size rule.
Can I travel if my pregnancy is high-risk?
Travel can be possible in the early second trimester if your condition is stable and your specialist agrees. The plan changes if you have placenta previa, preterm labour risk, high blood pressure that is hard to control, or twins. If travel is approved, carry records, identify a hospital at your destination, and avoid long stretches without moving your legs.
How often will I need scans and check-ups?
The schedule is individual. Some women attend monthly until 28 weeks, then every two weeks, then weekly from 36 weeks. Others need more frequent visits. Growth scans and non-stress tests are added when indicated. Your team will give you a written plan so you can organise work and family support.
Will my baby be healthy if the pregnancy is high-risk?
Most babies in high-risk pregnancies are born healthy, particularly when surveillance is consistent and treatment plans are followed. The purpose of high-risk care is to find and fix problems early and to choose the best time and place for birth if complications arise.
Can I still exercise?
Light to moderate activity is often encouraged, but some conditions require temporary restriction. Your specialist will advise you. If exercise is allowed, choose steady movement like walking or swimming and avoid overheating. Stop and seek advice if you feel unwell.
A note from Dr. Neha Lalla
Labels can feel daunting, but a high-risk pregnancy is simply a pregnancy that deserves extra care. With clear information, respectful communication, and careful monitoring, we guide most families to a safe birth. My role as a high-risk pregnancy specialist in Dubai is to personalise your plan, coordinate maternal fetal medicine support when needed, and be available for your questions so you feel informed at every step.
Conclusion and next steps
High-risk pregnancy care is not about alarms. It is about attention. By learning the signs of high-risk pregnancy, engaging early with specialist services, and following a structured plan, you can reduce the chance of pregnancy complications and protect your baby’s well-being.
If you have risk factors, new symptoms, or simply want an expert review of your plan in Dubai, book a consultation with Dr. Neha Lalla. Together, you can map out surveillance, discuss maternal fetal medicine input, and prepare for a birth that is safe, calm, and centred on your goals.


